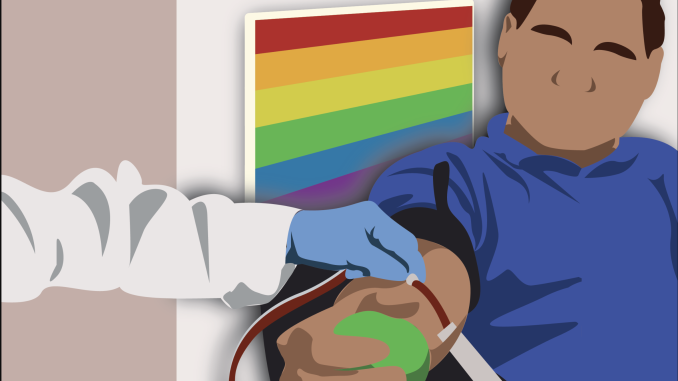
In May 2021, Dean Bruce, a sophomore public relations major, attempted to donate blood at a blood drive in Raleigh, North Carolina, amid a decrease in nationwide blood donations and supply due to the COVID-19 pandemic. However, they were rejected from donating due to their sexual history, which was a deeply painful experience, they said.
“It was sad,” Bruce said. “It was depressing to be like, ‘Oh, this is the way that we’re still operating.’”
Until last Friday, the U.S. Food and Drug Administration has prohibited any male who has had sexual contact with another male from donating blood for three months because it puts the donor at risk of becoming infected with HIV, according to the American Red Cross. Bruce identifies as nonbinary and bisexual, and, at the time, they were partaking in sexual relationships with male partners as a biological male.
However, this National Blood Donor Month, the FDA announced a proposal to assess blood donor eligibility through individual, gender-inclusive risk screenings to prevent HIV from entering the country’s blood supply after decades of criticism for a homophobic and outdated policy.
Although the FDA is taking a step toward inclusivity, this proposal still targets men who have sex with men by only restricting donors who have had anal sex, not vaginal sex, for an extended abstinence period. The FDA must continue to reevaluate the blood donor restrictions targeting MSM to stop the discriminatory misconception that gay men are the biggest spreaders of HIV.
This new policy will allow MSM in monogamous relationships to donate blood without abstaining from sex, but any person who has had anal sex with any new or multiple sexual partners in the past three months would be deferred from donation. Additionally, it will prevent people taking pre-exposure prophylaxis or post-exposure prophylaxis, medications to prevent HIV infections, from donating blood, according to the FDA.
The restriction previously singled out MSM while ignoring other people that partake in sexual activities that could increase the risk of HIV, like straight men and women who have unprotected sex. Now, it only focuses on anal sex, which is still more commonly a sexual experience between MSM than heterosexual couples.
Although MSM are still disproportionately affected by AIDS, 22 percent of HIV diagnoses, which can lead to AIDS if not treated, were acquired through heterosexual contact in the United States in 2020, according to the Department of Health and Human Services.
Any unprotected sexual activity could put a potential donor at risk for HIV, so MSM shouldn’t be singled out with restrictions placed only on anal sex.
“I consider a person’s sexuality an unalterable trait, while behavior is alterable,” said Billie Swiggard, an attending physician with specialty training in infectious diseases at the Mazzoni Center, an LGBTQ health organization on Bainbridge and Broad Streets.
Sexually active people who take preventative measures, like PrEP or consistent condom use, or can present a negative HIV test should be able to donate blood without deferral. PrEP, when taken properly, reduces the risk of contracting HIV through sex by about 99 percent, according to the Centers for Disease Control and Prevention.
Additionally, all donated blood is tested for evidence of infectious disease pathogens, including HIV, according to the CDC. The window period for contracting the disease and a positive test is between 10 and 33 days with a nucleic acid test, which can be used to test donated blood samples.
With a nucleic acid test, the deferral period for people who have recently participated in high-risk behavior could reasonably be shortened to one month instead of three months.
MSM have been able to donate blood three months after their last sexual encounter since April 2020, down from the previous FDA rule of one year. Before that, there was a lifetime ban on all MSM donors since 1983, when the AIDS crisis was at its peak, NBC News reported.
“It really is a kind of throwback to the late 80s, early 90s with the HIV epidemic, and it didn’t make sense then, and it really doesn’t make sense now,” said Sarah Bass, a social and behavioral sciences professor and the director of the Risk Communication Laboratory in the College of Public Health, about the recently-adjusted guidelines.
This National Blood Month, the FDA must continue to evaluate its recently-released proposal before enforcing the new guidelines to fully remove homophobic restrictions from blood donation in the United States.


Be the first to comment